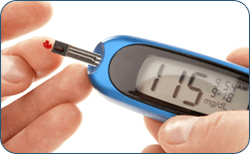
 Diabetes mellitus is a condition in which the amount of glucose (sugar) in the blood is too high because the body cannot use it properly.
Diabetes mellitus is a condition in which the amount of glucose (sugar) in the blood is too high because the body cannot use it properly.
Glucose comes from the digestion of starchy foods such as bread, rice, potatoes, chapatis, yams and plantain, from sugar and other sweet foods, and from the liver which makes glucose.
Insulin is vital for life
It is a hormone produced by the pancreas, which helps the glucose to enter the cells where it is used as fuel by the body. The main symptoms of untreated diabetes are increased thirst, going to the loo all the time – especially at night, extreme tiredness, weight loss, genital itching or regular episodes of thrush, and blurred vision.
Type 1
(insulin dependent) diabetes develops if the body is unable to produce any insulin. This type of diabetes usually appears before the age of 40. It is treated by insulin injections and diet, and regular exercise is recommended.
Type 2
(non insulin dependent) diabetes develops when the body can still make some insulin, but not enough, or when the insulin that is produced does not work properly (known as insulin resistance). This type of diabetes usually appears in people over the age of 40, though often appears before the age of 40 in South Asian and African-Caribbean people. It is treated by diet and exercise alone or by diet, exercise and tablets or by diet, exercise and insulin injections.
The pancreas
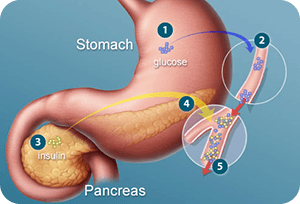 The pancreas is a long, soft organ that lies transversely along the posterior abdominal wall, posterior to the stomach, and extends from the region of the duodenum to the spleen. In people with diabetes, the pancreas does not produce enough insulin, or the insulin it produces does not work properly.
The pancreas is a long, soft organ that lies transversely along the posterior abdominal wall, posterior to the stomach, and extends from the region of the duodenum to the spleen. In people with diabetes, the pancreas does not produce enough insulin, or the insulin it produces does not work properly.
Simply put, diabetes is the result of a deficiency of insulin, which is found in the endocrine tissue of the pancreas. Traditional treatment of diabetes includes the regulated use of insulin and/or oral medications, in addition to proper diet and exercise.
Introduction
To keep well and healthy, everyone with diabetes needs good and regular healthcare. The early detection, treatment and continued control of your diabetes is very important as this will reduce your chances of developing the serious health problems (complications) linked to diabetes, such as heart disease, kidney disease and blindness.
What you should expect from the National Health Service (NHS)
You should receive all health services without discrimination because of age, lifestyle, gender, ethnicity, class, religion, disability, sexuality or your ability to pay.
The NHS should:
- Treat you with respect and dignity
- Tell you how to contact your diabetes care team
- Treat you with skill and care, and regularly review your clinical needs
- Answer any questions about the quality of the services you are getting
- Provide an interpreting service if English is not your first language, or if you have a sensory impairment or learning difficulties
- Provide information about local health services and how to contact them
- Keep you up to date about your diabetes, its care and treatment (and give you access to a second opinion subject to the agreement of your own GP or consultant)
Diabetes – What care you should expect from your diabetes care team
To achieve the best possible diabetes care, you need to work together with healthcare professionals as equal members of your diabetes care team. It is essential that you understand your diabetes as well as possible so that you are an effective member of this team.

You need to discuss with your consultant or GP the roles and responsibilities of those providing your diabetes care and to identify the key members of your own diabetes care team.
Members in your diabetes care team
- Yourself
- Consultant physician/diabetologist
- GP
- Diabetes specialist nurse (DSN)
- Practice nurse
- Dietitian
- Optometrist/ophthalmologist
- Podiatrist/chiropodist
- Psychologist
- Medical specialists
- Pharmacist
You may see some members of your diabetes care team more often than others
Changes in the delivery of diabetes care
There are several new initiatives which aim to make best practice the norm wherever you receive your care. The initiatives have also been set up to reduce the medical complications associated with diabetes.
Wherever you go for your diabetes care, it is important that you are getting the recommended standard of care. In England and Wales there are new national service frameworks for diabetes (National Service Framework for Diabetes) and in Scotland there is the Scottish Diabetes Framework. Similar decisions for a diabetes framework are being taken in Northern Ireland.
These frameworks set out standards of care which will be implemented over the next few years in order to bring about improvements to diabetes care throughout the UK.
Areas considered by the frameworks include:
- The prevention and early identification of Type 2 diabetes
- Empowering and educating people
- Improving clinical care, including care plans and patient held record
- Early detection and management of diabetes-related complications
- Better treatment during admission to hospital
- Integrated health and social care for those who need it
When you have just been diagnosed, your care team should:
- Give you a full medical examination
- Work with you to agree a care plan which suits you and includes diabetes management goals – this may take the form of a record for you to keep
- Arrange for you to talk with a diabetes specialist nurse (or practice nurse) who will explain what diabetes is and discuss your individual treatment and the equipment you will need to use
- Agree on a named healthcare professional to contact for support, advice or if you need more information
- Arrange for you to talk with a state registered dietitian, who will want to know what you usually eat, and will give you advice on how to fit your usual diet in with your diabetes – a follow-up meeting should be arranged for more detailed advice
- Tell you about your diabetes and the beneficial effects of a healthy diet, exercise and good diabetes control
- Discuss the effects of diabetes on your job, driving, insurance, prescription charges, and if you are a driver, whether you need to inform the DVLA and your insurance company
- Provide you with regular and appropriate information and education, on food and footcare for example
- Refer you to a structured education programme meeting national criteria
- Give you information about Diabetes UK services and details of your local Diabetes UK voluntary group
- Refer you to a psychologist should you need to discuss how to cope with the diagnosis/condition
Once your diabetes is reasonably controlled, you should:
- Have access to your diabetes care team at least once a year – in this session, take the opportunity to discuss how your diabetes affects you as well as your diabetes control
- Be able to contact any member of your diabetes care team for specialist support and advice, in person or by phone
- Have further education sessions when you are ready for them
- Have a formal medical annual review once a year with a doctor experienced in diabetes
On a regular basis, your diabetes care team should:
- Provide continuity of care, ideally from the same doctors and nurses. If this is not possible, the doctors or nurses who you are seeing should be fully aware of your medical history and background
- Work with you to continually review your care plan, including your diabetes management goals
- Let you share in decisions about your treatment or care
- Let you manage your own diabetes in hospital after discussion with your doctor, if you are well enough to do so and that is what you wish
- Organise pre and post pregnancy advice, together with an obstetric hospital team, if you are planning to become or already are pregnant
- Encourage a carer to visit with you, to keep them up to date on diabetes to be able to make informed judgements about diabetes care
- Encourage the support of friends, partners and/or relatives
- Provide you with educational sessions and appointments if you wish
- Give you advice on the effects of diabetes and its treatments when you are ill or taking other medication
Plus
If you are treated by insulin injections you should:
- Have frequent visits showing you how to inject, look after your insulin and syringes and dispose of sharps (needles). You should also be shown how to test your blood glucose and test for ketones and be informed what the results mean and what to do about them
- Be given supplies of, or a prescription for the medication and equipment you need
- Discuss hypoglycaemia (hypos): when and why they may happen and how to deal with them
If you are treated by tablets you should:
- Be given instruction on blood or urine testing and have explained what the results mean and what to do about them
- Be given supplies of, or a prescription for the medication and equipment you need
- Discuss hypoglycaemia (hypos): when and why they may happen and how to deal with them
If you are treated by diet alone you should:
- Be given instruction on blood or urine testing and have explained what the results mean and what to do about them
- Be given supplies of equipment you may need
- Be offered nutritional advice
Your responsibilities
 Effective care is normally achieved by teamwork, between you and your diabetes care team. Looking after your diabetes and changing your lifestyle to fit in with the demands of diabetes is hard work, but you’re worth it!
Effective care is normally achieved by teamwork, between you and your diabetes care team. Looking after your diabetes and changing your lifestyle to fit in with the demands of diabetes is hard work, but you’re worth it!
You will not always get your care right; none of us does, but your diabetes care team is there to support you. Ask questions and request more information especially if you are uncertain or worried about your diabetes and/or treatment. Remember the most important person in the team is you.
The following list of responsibilities is given to help you play your part in your own diabetes care.
It is your responsibility:
- To take as much control of your diabetes on a day-to-day basis as you can. The more you know about your own diabetes, the easier this will become
- To learn about and practice self-care which should include dietary education, exercise and monitoring blood glucose levels
- To examine your feet regularly or have someone check them
- To know how to manage your diabetes and when to ask for help if you are ill, eg chest infection, flu or diarrhoea and vomiting
- To know when, where and how to contact your diabetes care team
- To build the diabetes advice discussed with you into your daily life
- To talk regularly with your diabetes care team and ask questions
- To make a list of points to raise at appointments, if you find it helpful
- To attend your scheduled appointments and inform the diabetes care team if you are unable to do so
- To carry some form of identification about your diabetes status
Diabetes – What care you should expect in hospital
You may be admitted to hospital for reasons related or unrelated to your diabetes. In hospital, responsibility for the management of diabetes should be shared between you and the health professionals. Good diabetes control is important for a speedy recovery and early discharge.
You should:
- Receive a full explanation of your treatment during your stay in hospital and have the opportunity to discuss any particular worries. If you do not receive an explanation, ask for it
- Inform the ward team of your usual diet, tablets or insulin treatment. Bring your own supplies with you. If they are removed for safe keeping, make sure that they are returned to you at the end of your stay
- Have access to the hospital diabetes care team – doctor, nurse, state registered dietitian and chiropodist. Make sure they know you have been admitted
- Be allowed to discuss your diabetes so you can manage some aspects of it yourself, such as blood/urine monitoring and injections, if you wish. However, the staff may need to check your technique and results and they may need to do additional tests of their own
- If you are treated by insulin, expect that it may be given via a glucose/insulin drip into a vein if for some reason you are not allowed to eat or drink. If you are having anaesthetic an anaesthetist will arrange care of your diabetes during and immediately following the operation
- If you are treated by tablets, be prepared that your treatment may need to be changed while in hospital, which may involve being transferred from tablets to insulin during your stay
- Expect to be able to use your own emergency supplies of biscuits, sugary drinks, fruit or glucose tablets to treat hypoglycaemia. If you are on insulin or sulphonylurea tablets you should bring these supplies with you. If you do experience a hypo, inform your nurse or doctor
- Expect to be informed and consulted about any changes in your treatment or diet which may be necessary during your stay in hospital. For example, people with Type 2 diabetes are sometimes temporarily treated with injections of insulin while in hospital. This is because their illness or operation has upset their diabetes control
If you are unsure about the treatment or diet you are receiving in hospital, speak to your doctor, nurse or state registered dietitian.
What you should do if you have a complaint
It is important to discuss your complaint with those providing you with your care (eg GP or hospital staff). Each general practice and hospital will have internal procedures to deal with complaints in the first instance, through local resolution. If you are unable to complain yourself, a relative or friend can complain for you.
If this does not solve the problem and you live in England, you should contact your Patient Advice and Liaison Service (PALS) staff at your NHS trust hospital or primary care trust. They may be able to help resolve your concerns or can provide you with information and advice about how to complain formally, and refer you to an independent complaints advocacy service (ICAS). This service will also provide interpreters for the complaints process. If you live in Scotland, Wales and Northern Ireland, you should contact your Community Health Council (CHC) for advice about the complaints procedure.
If you are still dissatisfied after these procedures, ask for the Health Service Ombudsman to investigate. Contact details for CHCs and PALS can be found in your phone book or at your surgery, hospital, or Citizens Advice Bureau.
Further information
National Service Frameworks (NSF)
England
For copies of the National Service Framework for Diabetes: Standards and Delivery strategy for England, contact:
Department of Health
Email diabetes.nsf@doh.gsi.gov.uk
or log on to: www.doh.gov.uk
NSF patient information Living with diabetes your future health and wellbeing is downloadable from the Diabetes UK website:
(www.diabetes.org.uk) or is available from the Department of Health (see above).
For copies of the Scottish Diabetes Framework contact:
CRAG
NHS Quality Improvement Scotland Elliott House
8-10 Hillside Crescent
Edinburgh EH7 5EA
or log on to: www.show.scot.nhs.uk
